Overview
This guideline covers diagnosing and managing venous thromboembolic diseases in adults. It aims to support rapid diagnosis and effective treatment for people who develop deep vein thrombosis (DVT) or pulmonary embolism (PE). It also covers testing for conditions that can make a DVT or PE more likely, such as thrombophilia (a blood clotting disorder) and cancer. It does not cover pregnant women.
See the MHRA advice on warfarin and other anticoagulants – monitoring of patients during the COVID-19 pandemic, which includes reports of supratherapeutic anticoagulation with warfarin.
Last reviewed: 2 August 2023
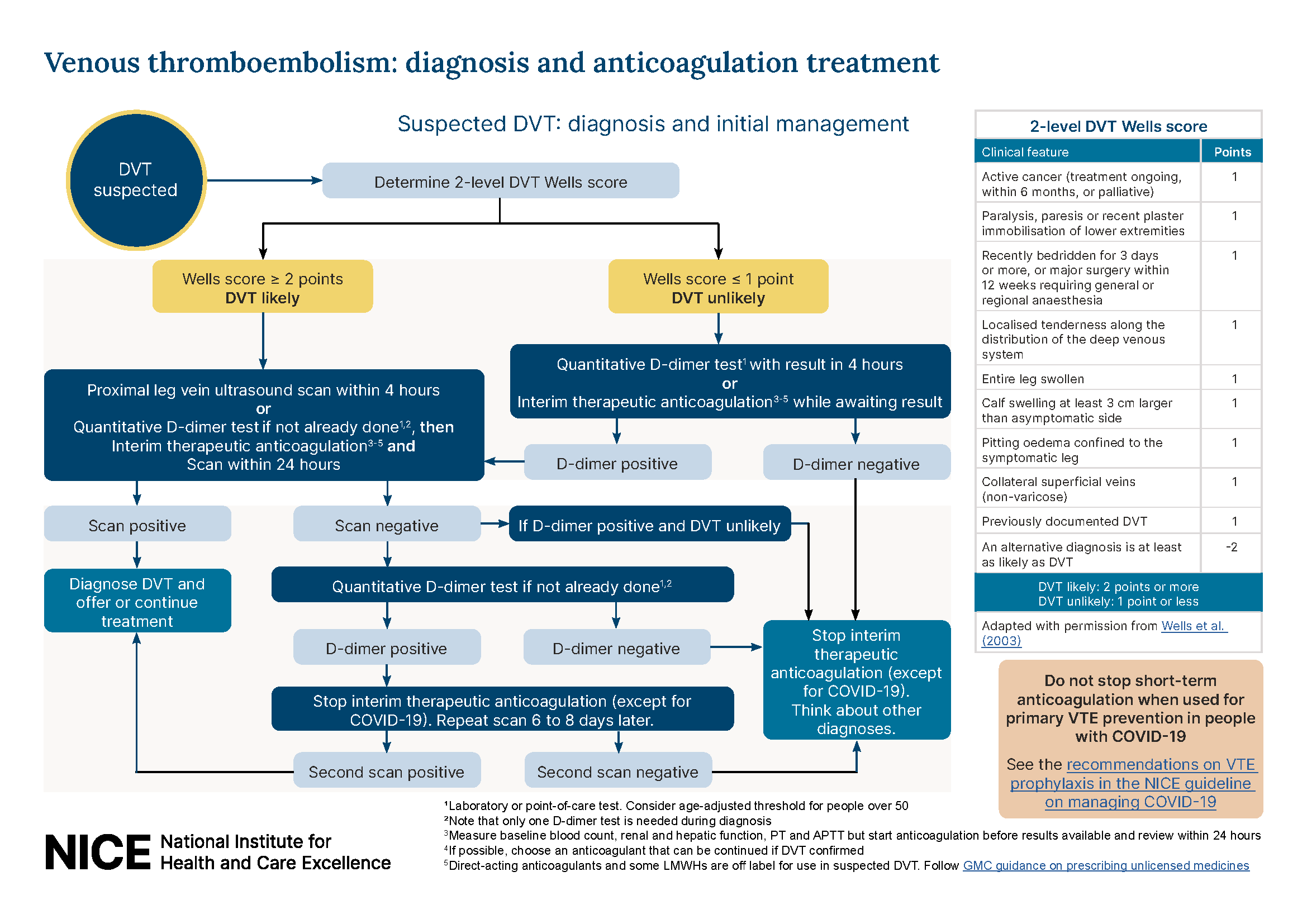
We updated recommendations on the use of Wells score and D-dimer in the diagnostic pathways for pulmonary embolism and deep vein thrombosis, following a review of the evidence for people with COVID-19. We also clarified the recommendation on the use of the pulmonary embolism rule-out criteria (PERC). For more details, see the update information.
This guideline updates and replaces NICE guideline CG144 (June 2012).
Next review: This guideline will be reviewed if there is new evidence that is likely to change the recommendations.
How we prioritise updating our guidance
Decisions about updating our guidance are made by NICE’s prioritisation board. For more information on the principles and process, see NICE-wide topic prioritisation: the manual.
For information about individual topics, including any decisions affecting this guideline, see the summary table of prioritisation board decisions.
Recommendations
This guideline includes recommendations on:
- diagnosing and managing suspected DVT and PE
- outpatient management of low-risk PE
- anticoagulation treatment for suspected or confirmed DVT or PE
- long-term anticoagulation for secondary prevention
- information and support for people having anticoagulation treatment
- thrombolytic therapy, inferior vena caval filters, investigations for cancer and thrombophilia testing
Who is it for?
- Commissioners and providers of venous thromboembolism services
- Healthcare professionals in primary, secondary and tertiary care
- Adults (18 and over) with suspected or confirmed DVT or PE, their families and carers
- First-degree relatives of people with inherited thrombophilia or other venous thromboembolic diseases
Guideline development process
How we develop NICE guidelines
Your responsibility
The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals and practitioners are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or the people using their service. It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian.
All problems (adverse events) related to a medicine or medical device used for treatment or in a procedure should be reported to the Medicines and Healthcare products Regulatory Agency using the Yellow Card Scheme.
Local commissioners and providers of healthcare have a responsibility to enable the guideline to be applied when individual professionals and people using services wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with complying with those duties.
Commissioners and providers have a responsibility to promote an environmentally sustainable health and care system and should assess and reduce the environmental impact of implementing NICE recommendations wherever possible.