Impact on NHS workforce and resources
This updated NICE guideline on chronic obstructive pulmonary disease (COPD) has been reviewed for its potential impact on the NHS workforce and resources.
Recommendations likely to have an impact on resources
The guideline covers diagnosing and managing COPD. The recommendations that are most likely to have a substantial resource impact are:
- Recommendation 1.2.11, which recommends prescribing dual therapies for some people with newly diagnosed COPD
- Recommendation 1.2.88, on criteria for referring patients for possible lung volume reduction surgery.
Context
Around 80,000 people are newly diagnosed with COPD in England each year, and in 2015/16 there were 262 finished consultant episodes for lung volume reduction surgery.
Services for people with COPD are commissioned by CCGs. Providers are NHS hospital trusts and general practitioners.
Resource impact
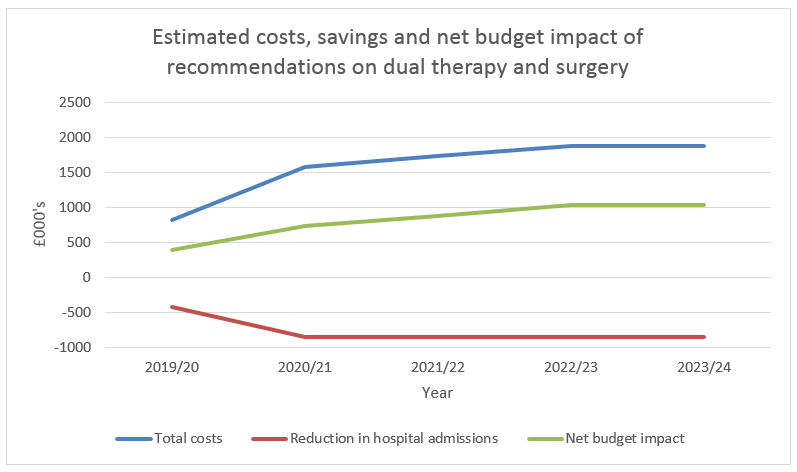
We estimate that if these recommendations are implemented it will have the following resource impact:
- An increase in people taking dual therapy, and more people having surgery.
- Increased prescribing of dual therapies for people with newly diagnosed COPD, meaning they are less likely to be admitted with an acute exacerbation.
- Overall, a potential increase in costs, partly offset by savings in hospital admissions, although potential savings are more difficult to quantify. Any costs and savings would impact on CCGs.
The potential costs and savings
The table and graph show the estimated impact over the first 5 years.
| Recommendation |
2019/20 (£000) |
2020/21 (£000) |
2021/22 (£000) |
2022/23 (£000) |
2023/24 (£000) |
| Prescribing more dual therapies | 609 | 1,218 | 1,218 | 1,218 | 1,218 |
| Increase in lung volume surgery | 204 | 351 | 510 | 657 | 657 |
| Total costs | 813 | 1,569 | 1,728 | 1,875 | 1,875 |
| Reduction in hospital admissions | (426) | (852) | (852) | (852) | (852) |
| Net budget impact | 387 | 717 | 876 | 1,023 | 1,023 |
There could also be a small cost associated with an increase in MDT appointments.
Commissioners should be aware of the following:
- The savings estimated from implementing these recommendations – as per the analysis above – may not be as readily identifiable as the costs.
- Due to growing competition between manufacturers of inhalers, there is potential for inhaler unit costs to fall in the future, which would help to reduce the cost pressure from these recommendations.
Support to put the recommendations into practice
- NICE, NHS England and NHS Improvement support improvements in the diagnosis and management of COPD.
- As part of the NHS Long term plan, published in January 2019, over the next 10 years the NHS will be targeting investment in improved treatment and support for those with respiratory disease by:
- doing more to support early detection and diagnosis of respiratory problems including via the development of primary care networks. More staff in primary care will be trained and accredited to provide the specialist input required to interpret spirometry results
- expanding pulmonary rehabilitation services to increase access to support a wider group of patients with rehabilitation and self-management
- supporting people with respiratory disease to receive and use the right medication. Pharmacists in primary care networks will undertake a range of medicine reviews, including educating patients on the correct use of inhalers.
| The guideline resource and implementation panel |
|
The guideline resource and implementation panel reviews NICE guidelines that have a substantial impact on NHS resources. By ‘substantial’ we mean that:
Panel members are from NICE, NHS England, NHS Improvement, Health Education England and when appropriate Public Health England and Skills for Care. Topic experts are invited for discussions on specific topics. The panel does not comment on or influence the guideline recommendations outside of NICE’s usual consultation processes and timelines. |
This page was last updated: