Impact on NHS workforce and resources
This NICE guideline on abortion care has been reviewed for its potential impact on the NHS workforce and resources.
Recommendations likely to have an impact on resources
The guideline covers care for women of any age (including girls and young women under 18) who request an induced abortion. It aims to improve the organisation of services and make them easier for women to access. It includes recommendations on conducting abortions at different gestational ages, to ensure that women get the safest and most effective care possible, in line with their own choice. The recommendations that are most likely to have a substantial resource impact are:
- Recommendation 1.1.5 - Commissioners should work with providers to ensure abortion services have the capacity and resources to deliver the range of services needed with minimal delay.
- Recommendation 1.3.2 - Do not offer anti-D prophylaxis to women who are having a medical abortion up to and including 10+0 weeks’ gestation.
- Recommendation 1.7.1 - Consider abortion before there is definitive ultrasound evidence of an intrauterine pregnancy (a yolk sac) for women who do not have signs or symptoms of an ectopic pregnancy.
Context
Abortion is a common procedure. In 2018, around 200,000 women in England and Wales had an abortion. Almost all of these abortions were funded by the NHS, but 72% were performed by the independent sector.
Most abortions are carried out because the pregnancy was unintended, and the majority of procedures (80% of abortions in England and Wales in 2018) are conducted in the first 10 weeks of pregnancy. Abortion is a safe procedure and can be carried out medically (taking mifepristone followed by misoprostol) or surgically.
The trend in England and Wales over the past decade has been towards increasing use of medical abortion. In 2018, 71% of all abortions in England and Wales were medical, and this rises to 83% of abortions in the first 10 weeks of pregnancy.
In recent years, there have been changes in how and where abortion services are delivered. This has resulted in variation in the type and choice of procedures available across the NHS, for example, in the offer of local anaesthesia and sedation for a surgical procedure. In addition, the procedure used for medical abortion has been refined and women in the first 10 weeks (up to 9 weeks and 6 days) may now self-administer misoprostol at home. Furthermore, methods for checking whether a medical abortion has been successful have also been simplified. Some of these developments could significantly reduce costs to the NHS and be more acceptable to women.
Abortion services are commissioned by clinical commissioning groups. Providers are NHS services and independent providers. Contraception and family planning services are commissioned by local authorities and provided by GPs, community providers and NHS trusts.
Resource impact
We estimate that implementing these recommendations would have the following resource impact:
Costs
- In order to reduce delays in abortions some providers may need to invest in their services. In some regions this may mean installing a dedicated phone and booking system.
- In regions where fewer surgical abortions are currently provided, staff may need extra training and there may be a need for greater access to operating theatres in order to increase access to surgical abortions.
Savings
- A reduction in waiting times for an abortion. This will result in fewer surgical abortions overall and a corresponding increase in earlier medical abortions which have a lower tariff.
- An increase in earlier medical terminations may also lead to a reduction in outpatient appointments and diagnostic tests.
- A reduction in the number of women having rhesus status testing and anti-D prophylaxis.
- A reduction in the number of ultrasound scans.
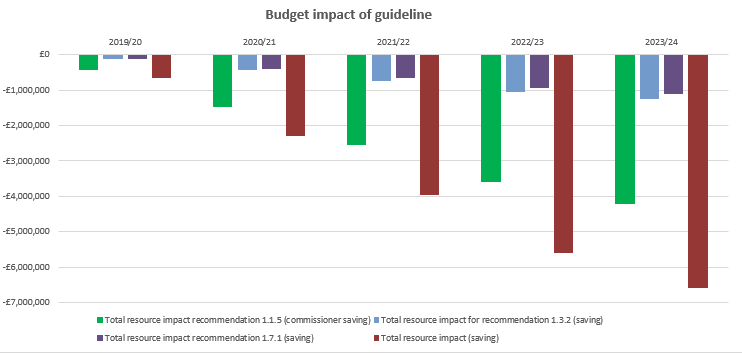
Costs and savings over the first 5 years
|
2019/20 |
2020/21 |
2021/22 |
2022/23 |
2023/24 |
|
| Implementation rate | 10% | 35% | 60% | 85% | 100% |
| Total resource impact recommendation 1.1.5 (commissioner saving due to minimal delays) (£m) | -0.4 | -1.5 | -2.5 | -3.6 | -4.2 |
| Total resource impact recommendation 1.3.2 (provider saving due to reduction in anti-D prophylaxis) (£m | -0.1 | -0.4 | -0.7 | -1.1 | -1.2 |
| Total resource impact recommendation 1.7.1 (commissioner saving due to reduced waiting times) (£m) | -0.1 | -0.4 | -0.7 | -0.9 | -1.1 |
| Savings for commissioners (£m) | -0.5 | -1.9 | -3.2 | -4.5 | -5.3 |
| Savings for providers (£m) | -0.1 | -0.4 | -0.7 | -1.0 | -1.2 |
| Total savings for England (£m) | -0.7 | -2.3 | -3.9 | -5.6 | -6.6 |
| Total saving per 100,000 population for commissioners (£000) | -1.0 | -3.4 | -5.8 | -8.2 | -9.6 |
| Total saving per 100,000 population for providers (£000) | -0.2 | -0.8 | -1.3 | -1.9 | -2.2 |
| Total saving per 100,000 population (£000) | -1.2 | -4.1 | -7.1 | -10.0 | -11.8 |
Budget impact of implementing the guideline
Support to put the recommendations into practice
- The Department of Health and Social Care integrated sexual health services guidance outlines how services and commissioners can collaborate to provide integrated provision. The guide highlights provision of rapid and easy access to open access reproductive health services including the full range of contraceptive services and supported referral to NHS funded abortion services, aligned to section 1.15 of the Abortion Care guideline.
- Abortion care is part of the Royal College of Obstetricians and Gynaecologists’ (RCOG) core curriculum (updated and published June 2019). All trainee obstetricians and gynaecologists will therefore receive training and will need to show they are able to provide this care.
- The RCOG also provides an advanced skills module on safe practice in abortion care for those wanting to specialise in abortion care. This module covers medical and surgical abortion up to 23+6 weeks’ gestation.
- The following changes may need to be made to current abortion service specifications to align with this guideline. Services should:
- be set up to allow self-referrals.
- be able to receive rapid referrals from non-NHS services, for example from sexual health services commissioned by local authorities.
- aim to provide assessment within 1 week of request and an abortion within 1 week of that assessment.
- offer a choice between medical and surgical abortion to all women before 24 weeks’ gestation. To help services discuss this choice with women, NICE have developed 2 decision aids (one for before 14 weeks’ gestation and one for between 14 and 23+6 weeks’ gestation).
| The guideline resource and implementation panel |
|
The guideline resource and implementation panel reviews NICE guidelines that have a substantial impact on NHS resources. By ‘substantial’ we mean that:
Panel members are from NICE, NHS England, NHS Improvement, Health Education England and when appropriate Public Health England and Skills for Care. Topic experts are invited for discussions on specific topics. The panel does not comment on or influence the guideline recommendations outside NICE’s usual consultation processes and timelines. |
This page was last updated: