More people are benefitting from NICE-recommended statins to reduce heart attacks and strokes
Around 5.3 million people in England were given a NICE-recommended statin or ezetimibe by their GP to help reduce their cholesterol during 2023/24, the largest number on record and almost 900,000 more than in 2022/23.

High cholesterol can contribute to the blood vessel blockages that cause heart attacks, strokes and other conditions. It also increases the overall risk of cardiovascular disease (CVD) which is responsible for over a quarter of all deaths in England, one death every four minutes on average. People living in the most deprived areas or with severe mental illness are at higher risk of CVD.
Adding a statin to lifestyle changes (such as stopping smoking, being more active and eating a better diet) reduces the chance of first CVD events happening in people at high risk and reduces the risk of further events if they do occur.
Cardiovascular disease is the biggest area where we can save lives over the next ten years.
The wider use of these tablets to lower cholesterol is a key part of our plans to help prevent thousands of heart attacks and strokes, reduce health inequalities, and make best use of NHS resources.
We have recommended statins at the most effective doses for preventing and treating CVD since 2014. NICE recommends ezetimibe as an alternative treatment when statins are not suitable. Ezetimibe is also one of several treatment options recommended for people who may need additional help in managing their cholesterol levels.
Improving and increasing early detection and treatment of CVD will help people live longer, healthier lives.
Statins are medicines that lower the level of cholesterol in the blood and are a proven treatment to reduce the risk of heart attacks and strokes.
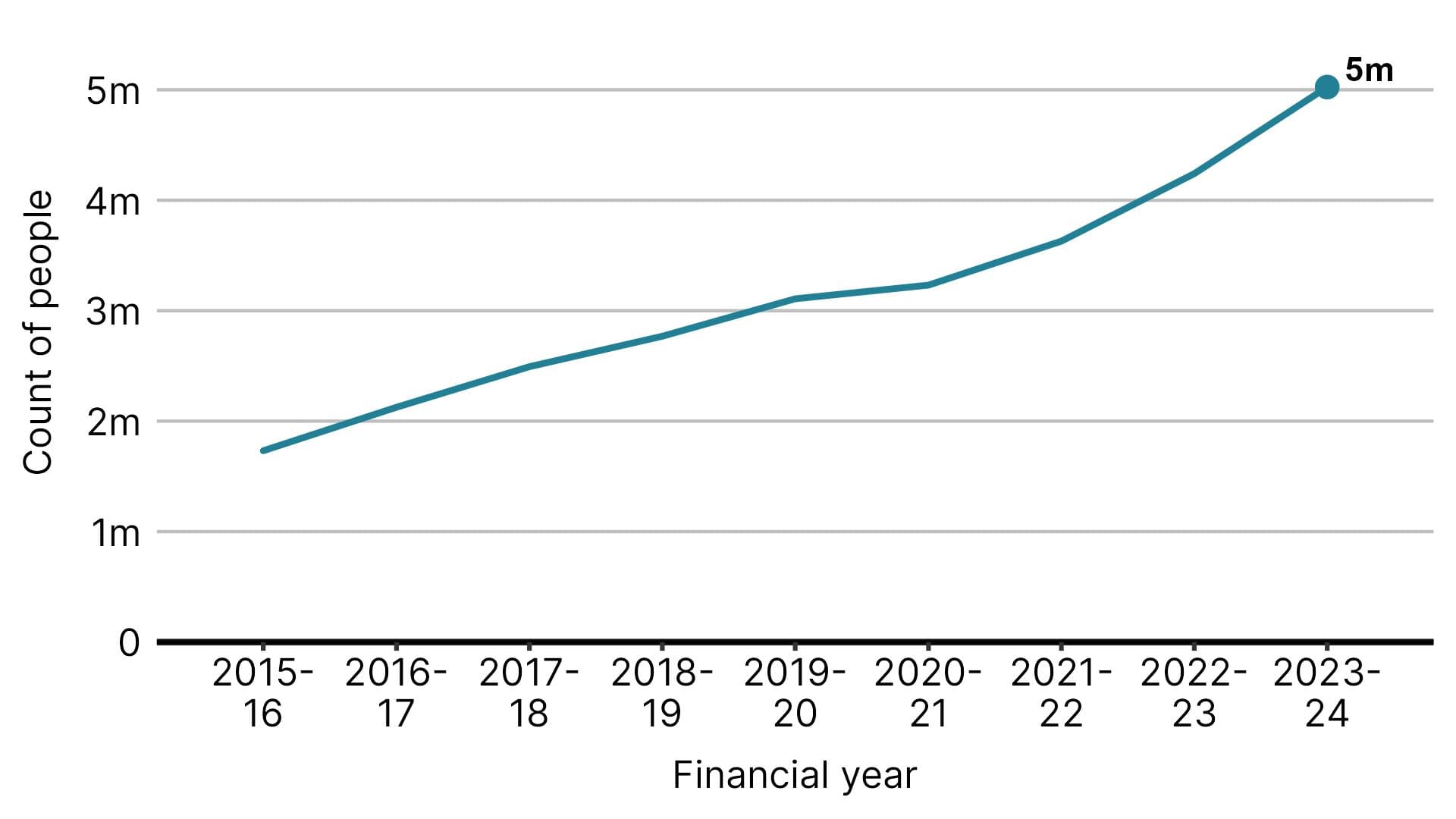
The number of people given NICE-recommended statins or ezetimibe in primary care in England increased 19% from 2022/23 to 2023/24 and has nearly tripled since 2015/2016.
Figure 1: Number of people dispensed atorvastatin 20mg, atorvastatin 80mg or ezetimibe 10mg in primary care in England, by financial year.
This is the largest annual increase since 2016/17. The increase coincides with the introduction of new cholesterol indicators in the GP Quality and Outcomes Framework (QOF) and the release last year of updated NICE guidance on cardiovascular disease.
Our updated guidance included, for the first time, a target for cholesterol levels that is estimated to benefit 2.1 million people with CVD. The QOF was recently updated to align with this target.
Uptake of the statin atorvastatin at NICE-recommended doses increased from 4.2 million people in 2022/23 to 5 million in 2023/24.
Figure 2: Number of people dispensed atorvastatin 20mg or atorvastatin 80mg in primary care in England, by financial year.
More than 400,000 people were dispensed ezetimibe 10mg—the NICE-recommended dose—in 2023/24. This is a 50% increase from the previous year and a 128% increase since 2015/16.
Figure 3: Number of people dispensed ezetimibe 10mg in primary care in England, by financial year.

57% of people given tablets to reduce their cholesterol by their GP were taking a NICE-recommended statin or ezetimibe, an increase from 26% in 2015/16.
Figure 4: Proportion of people on oral lipid lowering therapy who were dispensed a NICE-recommended statin or ezetimibe in primary care in England.

Colin Wilkinson, a lay committee member for our latest guideline on cardiovascular disease, has high cholesterol and a family history of heart failure. He started taking atorvastatin 20mg last year. “I haven’t had any side effects, and my cholesterol has gone from quite high to quite low.”
Preventing heart attacks, strokes and deaths
Figures from CVD Prevent show that the proportion of people with known CVD, or at high risk of developing CVD, who are on cholesterol lowering treatment has increased year on year.
Among adults with CVD, 85% were on cholesterol lowering treatment in June 2024, up from 82% in June 2023.
Size of the Prize shows that thousands of heart attacks, strokes, and deaths could be prevented by taking medication to lower cholesterol. If 95% of adults with CVD were on cholesterol lowering treatment, around 17,300 cardiovascular events such as strokes and heart attacks, and 2,000 deaths could be avoided.
More people on medication does mean higher treatment costs, but this is offset by savings from fewer heart attacks and strokes, and lower healthcare costs associated with these life-threatening events.
Mr Wilkinson plans to take statins long-term: “I understand that for somebody who is not taking any treatment, the idea of taking daily medication to prevent something from happening can seem a bit odd, but it’s better to take one pill a day than to have a heart attack or a stroke.
“Knowing that these medications are safe and save lives made it a simple decision for me.”
Increasing take-up
NHS England, NICE and other system partners have worked with pharmacists and GP services to increase awareness of the recommended treatment options along with ways to support healthier lifestyle choices by their patients.
This work has also looked to help GPs review existing prescriptions to make sure that people are on the right dose of medication to keep their cholesterol within the recommended levels.
Professor Benger said: “Our useful and useable guidance for the prevention of CVD is an important tool for both GPs and patients. It covers lifestyle changes and treatment options, including statins, and there is also a patient decision aid to help guide and inform conversations on the choices available.”
Janice Craig, Medicines Optimisation Lead Pharmacist for Buckinghamshire, Oxfordshire and Berkshire West Integrated Care Board (BOB ICB) said: “We have worked with primary care healthcare professionals to highlight the range of cholesterol treatments available and how they can help their patients better understand their risk factors and manage their cholesterol levels through treatment plans more effectively.”
Dr Heike Veldtman, GP and CVD Lead for BOB ICB added: “We have worked closely with the Health Innovation Network (HIN) and made a particular effort to reach people who might be at risk of CVD and not yet receiving help. The HIN has created leaflets, posters and videos. We have shared this far and wide, from being played in GP surgeries to mental health teams. We have translated leaflets into other languages spoken in our area.”
We have also recommended cholesterol lowering treatment at progressively lower levels of cardiovascular risk and in specific higher-risk subgroups. The QOF has helped encourage and support ongoing improvements in CVD care.
Alongside this there is now less concern from clinicians and the public about statin safety than there has been in the past.
“I think the biggest improvement is in clinicians’ appreciation of how important and what a big difference improving cholesterol management will make to the patient's outcome,” said Dr Heike.
Ms Sara Hafidh, Advanced Clinical Practitioner and Lead Pharmacist in Wakefield and Pontefract & Knottingley Primary Care Networks (PCNs), agrees that shared decision-making is a key part of the process: “The approach is patient-centred, patient-specific, based on their risk factors. Everything is a negotiation, getting the patient involved and giving them options. The more you involve them in their care, the more uptake you will have.”
Notes
1. Size of the Prize is a resource produced by UCLPartners.